INTRODUCTION Dizziness has a high incidence worldwide, and the impact of vestibular disease on quality of life has been increasingly investigated. Many patients with dizziness restrict their daily activities and leisure in order to reduce the risk of onset of unpleasant and frightening symptoms, as well as to avoid the social embarrassment and stigma that these symptoms may cause (1).
Benign paroxysmal positional vertigo (BPPV) is a disease with a high incidence worldwide, and can be regarded as the most frequent vestibular disease (2). There are few studies correlating BPPV and Meniere's disease (MD) and their combined influence on the quality of life of patients (3, 4). Simultaneous diagnosis of BPPV and MD may worsen symptoms of dizziness and thus worsen the quality of life, because the discomfort caused by these symptoms can significantly change the ability of patients to perform their usual tasks (4).
Among existing evaluation instruments, the Dizziness Handicap Inventory (DHI) is an internationally validated instrument. This questionnaire assesses patients' perception of the effects of the disabling vertigo on their quality of life, including the physical, emotional, and functional aspects. It is important to assess the individual's condition at the beginning of treatment and to monitor the evolution of the disease course (1) (Chart 1).
Treatment options for vertigo patients include medications, vestibular rehabilitation (VR) and, more rarely, surgical procedures (5). VR has been used as a strategy for the treatment of vestibular disorders because its goals are to provide security to the patient and integrate them into their social environment. VR aims to promote visual stabilization, improve static and dynamic balance, decrease sensitivity during head movement, and improve the overall function of the patient via proprioceptive and vestibular visual stimulation maneuvers (6).
The objective of this study was to evaluate the pre- and post-VR quality of life of patients with MD-associated BPPV by using the Brazilian version of the DHI as an evaluation tool.
METHODThe study was approved by the Ethics in Research on Humans Foundation Regional University of Blumenau (FURB), under protocol 180/09. The sample consisted of 12 patients of both genders with a diagnosis of Meniere's disease associated with benign paroxysmal positional vertigo (BPPV) of the posterior canal, who were seen at the ENT clinic during the period from October to December 2009. Inclusion criteria were as follows: clinical diagnosis of Meniere's disease with complementary electrocochleographic findings, presence of nystagmus triggered by Dix Hill Pike maneuvers and lateral placement test identified under the guidance of videonystagmography, no treatment initiation or maintenance during the period between surveys, agreement to undergo surgery to the ear, and agreement to signing a consent form. We excluded patients with signs and symptoms of vestibular central origin, those with musculoskeletal abnormalities that impair the performance of the maneuvers (diagnostic and therapeutic), individuals who began vestibular rehabilitation before completing the questionnaire, and patients undergoing vestibular rehabilitation lasting less than 5 sessions, considering the research period.
The sessions were held once a week individually, with each session lasting 1 hour. VR started with the canalith repositioning maneuver of Epley, where the individual sitting on the table adopts a supine position and the therapist rotates the head to the side of the affected labyrinth. After a minute, the head is rotated to the opposite side and the patient is instructed to stay in the same position for another minute, returning to a seated position at the end. This was followed by the Brandt and Daroff habituation exercises. From the seated position on the table, the patient adopts a lateral recumbent position (first on the side that causes the dizziness), maintains the position for 30 seconds or until the dizziness passes, changes to a lateral seated position, waits for the same time period, and then lies on the opposite side and waits for 30 seconds. Each patient was taught the exercises and instructed to repeat them at home 10-20 times a day. In addition, we performed the Cawthorne-Cooksey visual exercises consisting of up and down and side-to-side eye movements as well as extension of an arm and focusing on the finger as it approaches and moves away from the face. All movements were repeated 20 times, starting slowly and becoming progressively faster, with the patient sitting or lying down. In another exercise, with the individual sitting or standing, only the head moved forward and back, after a back and forth motion; these motions were first performed slowly and then rapidly, with eyes open and progressing to accomplishment of each movement and with eyes closed for 1 minute. The Brazilian version of the DHI was completed by participants before undergoing the first session of VR and after the last treatment session. Subjects were instructed to mark the item that best demonstrated their perception of the influence of vertigo on their quality of life at the time, with doubts addressed by the researchers present during the survey. The absence of symptoms/problems was marked "no," corresponding to 0 (zero), occasional presence of symptoms/problems was reported as "sometimes," and was scored as 2 points, and the presence of severe symptoms/problems was marked "yes," and amounted to 4 points. The minimum score of the questionnaire was 0 (zero) and the maximum was 100 points, with 7 items referring to physical aspects, 9 to functional aspects, and 9 to emotional aspects (7).
For data analysis, we first used the Shapiro-Wilk test of normality, proceeding with the Wilcoxon test for comparisons between samples before and after vestibular rehabilitation, and the Friedman test to compare the impact of physical, emotional, and functional scores after standardizing the values by calculating the percentage according to the maximum possible score to be obtained on each item. Spearman correlation was used to evaluate the relationship between aspects, the total score, and the characteristics of the sample test. All analyses were processed in 4.0 BioEstat considering significance at
p < 0.05.
RESULTSIn the stipulated period for data collection, 12 individuals fulfilled the criteria for inclusion and exclusion. There were 4 (33.33%) men and 8 (66.66%) women, all Caucasian, aged between 35 and 86 years (mean, 53.17 ± 15.75 years). Three (25%) were less than 40 years old, 6 (50%) were aged between 40 and 59 years, and 3 (25%) were aged 60 years or more (Table 1).
There was a significant reduction in all DHI values after VR, independent of the aspect. The median final values were 0 (zero) for the physical aspect, 1 for the emotional aspect, and 1 for the functional aspect, demonstrating the favorable impact of VR on the quality of life of our patients (Table 2). Generally, the score must be reduced by at least 18 after treatment to be indicative of benefit (1). In our series, 7 (58.33%) patients showed a reduction greater than 18 points, 5 (41.67%) did not show a reduction greater than 18 points, and 3 (25%) did not achieve a pre-VR score large enough to show such a reduction. In the evaluation of post-VR scores, 2 (16.6%) patients who had scores less than 18 pre-VR, despite showing an improvement in the aspects evaluated, did not show score reductions of the specified magnitude.
To compare the effects on the different aspects, the raw score values were normalized as percentage values, with 100% indicating the maximum score in every aspect. Next, we compared the pre- and post-VR scores. In the preoperative evaluation, we noted that the diseases had a greater impact on physical and functional aspects than on the emotional aspect. Although none of the aspects showed a predominant effect of VR, the differences in the pre- and post-VR values showed that VR had the greatest influence on the physical aspect (Table 3).
In the first evaluation (pre-VR), the correlation between the physical and functional aspects was moderately positive, and that between the emotional and functional aspects was strongly positive, indicating the interrelationship of these factors on quality of life of the volunteers, i.e., the functional aspect influences and is influenced by physical and emotional aspects. Post-RV, these correlations were not observed. However, analysis of the difference (pre - post) showed a weak positive correlation between the emotional and functional aspects (Table 4).
In the pre- and post-VR analyses, there was a lack of correlation between age and gender with the DHI scores, indicating that the results of the VR were not affected by these characteristics (Table 5).
It should be noted that the sample size did not allow generalization of the results; however, considering the results, the importance of VR is evident. In another study with 15 subjects who were diagnosed as having BPPV associated with Ménière's disease, the physical aspect was the most affected (4), but there are few studies analyzing both conditions together and using VR for the treatment of this combination.
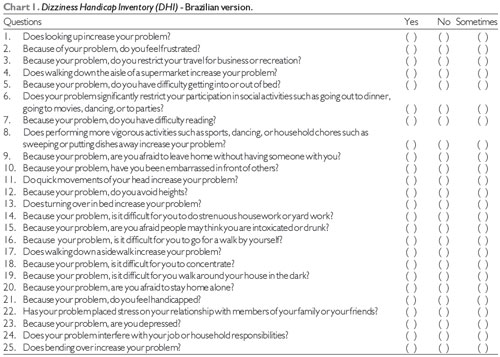
Legend: Physical aspects - Questions 1, 4, 8, 11, 13, 17 and 25; Functional aspects - Questions 3, 5, 6, 7, 12, 14, 16, 19 and 24, Emotional aspects - Questions 2, 9, 10, 15, 18, 20, 21, 22 and 23. Each YES answer = 4 points; SOMETIMES = 2 points; NO = 0 points. The final score is the sum of points obtained in all aspects.
Regarding gender, there was a predominance of women (75%) in the sample, which agrees with previous studies that found a prevalence of dizziness and BPPV in 61.3% to 62.5% of female patients (8, 9, 10). Some authors suggest that the variations in natural hormones in women could be related to this increased incidence, but did not elucidate this theory (11). As for Meniere's disease (MD) alone, there are reports of an equal distribution between genders (12). The most prevalent age group in this study also coincides with the findings obtained by other authors, who indicated that 48% to 60% of subjects were between 41 and 60 years of age (4, 7).
All individuals in the sample were diagnosed with MD and associated BPPV. Other studies have also reported the coexistence of these 2 diseases, with patients initially presenting symptoms of MD followed by symptoms of BPPV (13, 14). One hypothesis for this relationship between the 2 diseases is the possible release of otoconia by damage to the utricle by endolymphatic hydrops and hypertension (3).
The DHI-Brazilian version was used to assess the impact of VR on the quality of life of patients and, based on the significant score decrease in most patients, it is argued that VR is favorable for these patients. The dizziness and other symptoms that often accompany vestibular disorders may manifest during social, familial, and professional activities, thus causing physical, financial, and psychological distress to the patients (15,16,17) and necessitating interventions to eliminate or minimize these symptoms. Individuals end up restricting their head movements and activities to prevent vertigo, thereby imposing physical constraints that lead to functional loss and consequent emotional turmoil, which explains the damage caused by these disorders.
We found that pre-VR, the greatest impact was noted on the physical and functional aspects while after VR, the greatest influence was noted on the physical aspect, despite the reduction of the values in the functional and emotional aspects as well. It was noted that after the improvement in physical symptoms, individuals were able to resume their routine activities that were previously restricted due to dizziness or fear of symptoms, and this improvement consequently improved functional and emotional aspects, which are dependent on the physical aspects. This result contrasts the results of a previous study (18), where a sample of 6 patients, aged 43-70 years, with complaints of dizziness and tinnitus showed no significant improvement in the functional and emotional aspects and no improvement in the physical aspect after VR.
It should be noted that apart from vertigo, some individuals had age-related comorbidities (such as osteoarthritis and osteoporosis), which by itself has limited some of the emotional issues such as fear of high places and fear of being alone at home or going out unaccompanied. Therefore, it is likely that the answers to these questions were influenced by comorbidities, so it is not possible to separate them from the symptom of vertigo/dizziness. This situation indicates that the analysis of the emotional aspect should be undertaken with care, because if the individual is unable to perform some physical activity for problems not related to dizziness, even after the improvement of vertigo, he/she will be unable to do the same.
The correlation between the physical and functional aspects and between emotional and functional aspects in pre-VR assessments demonstrates the interrelationship of these factors with the quality of life of individuals, i.e., the functional aspect influences and is influenced by the physical and emotional aspects. However, this effect appears to be greater when the symptoms are exacerbated by vertigo, since after VR, no such correlation was observed. The relationship between the functional and physical aspects is also highlighted in other studies, where the similar scores for these aspects were explained by the fact that in BPPV, onset of symptoms is closely related to certain positions or head movements, the relevant questions for which are contained in both aspects of IHL-Brazilian version (19, 20).
Similarly, studies involving individuals with MD associated with higher scores on the physical and functional aspects to the chronic nature of the disease with clinical manifestations floating, recurrent and lasting, that can compromise not only physical, but also the functionality of these patients (4, 21). In another study with 6 patients aged 43-70 years, the analysis of the DHI questionnaire after VR showed that patients experienced an improvement in functional and emotional aspects, although the difference was not significant (18). Furthermore, the relationship of the functional to the emotional aspects can be understood by the rationale that when there is improved functionality, the individual returns to his/her daily habits, accomplishing all movements restricted before the onset of vertigo. Thus, the individual becomes more confident with regard to leaving the house without company and can simply raise the head or turn over in bed without being afraid of triggering symptoms.
The results of VR were not affected by age and/or gender, similar to previous studies that indicate no relationship between improvement in patients with vertigo and after VR with these variables (20, 22). In this context, the geriatric population responds to treatment as well as a younger population, but most of the elderly patients require a greater number of treatment sessions to achieve the same result as the young (23). Moreover, other studies describe that age is not necessarily associated with loss of independence in activities of daily living, and therefore, it is not possible to relate the age-diminished ability with greater independence or improvement in vertigo after vestibular alteration (24). On the other hand, dizziness has a more detrimental effect on quality of life of elderly than in younger adults, according to studies with these populations (25, 26, 27, 28). Regarding gender, some authors report that the variable is not related to any advantage or disadvantage in relation to response to treatment (7), a fact verified by the results presented here. As individuals in the sample were out of the crisis period during the questionnaire analysis and underwent VR, the results discussed are restricted to perception of symptoms by individuals on a daily basis, whereas in vertigo, the symptoms are exacerbated.
Finally, we would like to point out the importance of multidisciplinary medical and physiotherapy in the diagnosis and treatment to achieve greater security and adherence to this treatment modality.
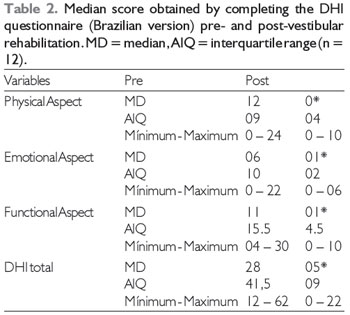
* p < 0.01 when compared to before.
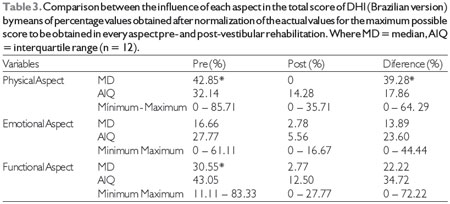
*p < 0.05 when compared to emotional aspect
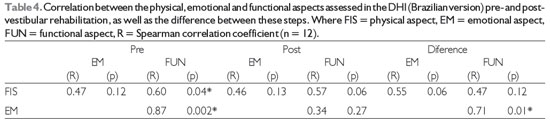
* where p < 0.05
The results obtained through the DHI Brazilian version show that the quality of life of patients with BPPV associated with MD improved after 5 sessions of VR in all aspects analyzed. We noticed that the diseases had a greater impact on the physical and functional aspects of quality of life before VR, with the highest rate of improvement noted in the perception of physical appearance after the therapy. Age and gender did not affect the response to treatment. Although the sample consisted of a small number of patients, the results obtained with VR were surprising and further studies need to be developed, especially involving the 2 pathologies. Moreover, the VR was well accepted by volunteers who showed increased enthusiasm and confidence with the evolution of treatment and reduction of symptoms.
REFERENCES1. Ganança FF, Castro ASO, Branco FC, Natour J. Interferência da tontura na qualidade de vida de pacientes com síndrome vestibular periférica. Rev. Bras. Otorrinolaringol. [online]. 2004, 70:94-101.
2. Ganança MM, Caovilla HH, Munhoz MSL, Ganança CF, Silva MLG, Serafini F, Ganança FF. Otimizando o componente farmacológico da terapia integrada da vertigem. Rev. Bras. Otorrinolaringol.[online]. 2007, 73:12-8.
3. Boaglio M, Soares LCA, Ibrahim CSMN, Ganança FF, Cruz OLM. Doença de Ménière e vertigem postural.Rev. Bras. Otorrinolaringol. [online]. 2003, 69:69-72.
4. Handa PR, Kuhn AMB, Schaffleln R, Ganança FF. Qualidade de vida em pacientes com vertigem posicional paroxística benigna e/ou doença de Ménière.Rev. Bras. Otorrinolaringol. [online]. 2005, 71:776-783.
5. Mantello EB, Moriguti JC, Rodrigues-Junior AL, Ferrioli E. Efeito da reabilitação vestibular sobre a qualidade de vida de idosos labirintopatas.Rev. Bras. Otorrinolaringol. [online]. 2008, 74:172-180.
6. Andre APR. Reabilitação vestibular da vertigem postural paroxística benigna de canal posterior em idosos. Ribeirão Preto, 2003, p.102, (Dissertação de Mestrado - Faculdade de Medicina de Ribeirão Preto/USP).
7. Moreira DA, Bohlsen YA, Momensohn-Santos TM, Cherubini AA. Estudo do Handicap em Pacientes com Queixa de Tontura, Associada ou Não ao Sintoma Zumbido. Arq. Int. Otorrinolaringol. São Paulo, 2006, 10:270-277.
8. Caovilla HH. Autorotação cefálica no diagnóstico da disfunção vestibular. RBMORLOtologia. 2000, 57:8-11.
9. Cusin FS, Silva SMR, Ganança CF. Achados na vestibulometria de pacientes com Vertigem Posicional Paroxística Benigna submetidos à Manobra de Epley. Acta ORL [online]. São Paulo, 2006, 24:69-74.
10. Koga KA, Resende BA, Mor R. Estudo da prevalência de tontura/vertigens e das alterações vestibulares relacionadas à mudança de posição de cabeça por meio da vectoeletronistagmografia computadorizada. Rev CEFAC. São Paulo, 2004, 6:197-202.
11. Bittar RSM. Sintomatologia auditiva secundária à ação dos hormônios. Femina. São Paulo, 1999, 27:739-741.
12. Fetter M. Disfunções do Sistema Vestibular. In: Herdman SJ. Reabilitação Vestibular. 2.ed. Barueri: Editora Manole, 2002, pp91-101.
13. Hughes CA, Proctor L. Benign paroxysmal positional vertigo. Laryngoscope. 1997, 107:607-613.
14. Gross EM, Ress BD, Viirre ES, Nelson JR, Harris JP. Intractable benign paroxymal positional vertigo in patients with Ménière's disease.Laryngoscope. 2000, 110:655-659.
15. Pedalini MEB, Bittar RSM. Reabilitação vestibular: uma proposta de trabalho. Pró-Fono, 1999, 11:140-144.
16. Knobel KAB, Pfeilsticker LN, Stoler G, Sanchez TG. Contribuição da reabilitação vestibular na melhora do zumbido: um resultado inesperado.Rev. Bras. Otorrinolaringol. [online]. 2003, 69:779-784.
17. Segarra-Maegaki JAS, Taguchi CK. Estudo do benefício da reabilitação vestibular nas síndromesvestibulares periféricas. Pró-Fono, 2005, 17:3-10.
18. Zeigelboim BS, Rosa MRD, Klagenberg KF, Jurkiewicz AL. Reabilitação vestibular no tratamento da tontura e do zumbido. Rev. Soc. Bras. Fonoaudiol. [online]. 2008, 13:226-232.
19. Castro ASO, Gazzola JM, Natour J, Ganança FF. Versão brasileira do Dizziness Handicap Inventory.Pró-Fono R. Atual. Cient. [online]. 2007, 19:97-104.
20. Patatas OHG, Ganança CF, Ganança FF. Qualidade de vida de indivíduos submetidos à reabilitação vestibular. Rev Bras Otorrinolaringol. [online]. 2009, 75:387-394.
21. Cunha F. Interferência da tontura na qualidade de vida em pacientes com doença de Ménière. São Paulo, 2003, p.85, (Tese de Mestrado - Universidade Federal de São Paulo).
22. Cohen HS, Kimball KT. Increased independence and decreased vertigo after vestibular rehabilitation. Otolaryngol Head Neck Surg., 2003, 128:60-70.
23. Bittar RSM, Pedalini MEB. Síndrome do desequilíbrio do idoso. Pró-Fono, 2002; 14:119-128.
24. Nishino LK, Granato L, Campos CAH. Aplicação do Questionário de Qualidade de Vida Diária em Pacientes Pré e Pós - Reabilitação vestibular. Arq. Int. Otorrinolaringol. 2008, 12:517-522.
25. Resende CR, Taguchi CK, Almeida JG, Fujita RR. Reabilitação vestibular em pacientes idosos portadores de vertigem posicional paroxística benigna. Rev. Bras. Otorrinolaringol. [online]. 2003, 69:535-540
26. Whitney SL, Wrisley DM, Marchetti GF, Furman JM. The effect of age on vestibular rehabilitation outcomes. Laryngoscope. 2002, 112:1785-90.
27. Simonceli L, Bittar RMS, Bottino MA, Bento RF. Perfil diagnóstico do idoso portador de desequilíbrio corporal: resultados preliminares.Rev. Bras. Otorrinolaringol. [online]. 2003, 69:772-777.
28. Gazzola JM, Perracini MR, Ganança MM, Ganança FF. Fatores associados ao equilíbrio funcional em idosos com disfunção vestibular crônica.Rev. Bras. Otorrinolaringol. [online]. 2006, 72: 683-690.
1) Physiotherapist. Physiotherapist, Blumenau/SC.
2) PhD from the University of São Paulo. Professor of Otorhinolaryngology in Regional University of Blumenau Foundation.
3) Master of Physiotherapy, Methodist University of Piracicaba. Professor of Kinesiology, Course of Physiotherapy in Regional University of Blumenau Foundation.
Institution: FURB - Fundação Universidade Regional de Blumenau. Blumenau / SC - Brazil. Mailing address: Dayra Dill Socher - Alameda Duque de Caxias, 145 - room 306 - Center - Blumenau / SC - Brazil - Zip code 89015-010 - Telephone: (+55 47) 3035-4640 - E-mail: ftdayra@yahoo.com.br
Article received in October 30, 2011. Article approved in July 22, 2012.