INTRODUCTIONThe chronic otitis media is still a prevalent disease in our area. The cases defined as cholesteatomatous chronic suppurative otitis media (CSOM) or non-cholesteatomatous (NCSOM), do not respond to clinical treatment, and are the most frequent causes for indication of mastoidectomy. The chronic otitis media is defined as an inflammatory process, infectious or not, focal or generalized in the middle ear. In the NCSOM there are irreversible alterations in the middle ear epithelium that manifest as chronic otorrhea and perforation of the tympanic membrane, which requires surgical treatment for the disease control.
The CSOM is defined as the presence of keratinized stratified squamous epithelium in any region of the middle ear and may be acquired or more seldom congenital. The cholesteatomas have characteristics of growth, migration and osseous erosion and are thus locally destructive, the only treatment is their full surgical removal, since there is no effective clinical treatment for eradication of the disease so far (1,2,3).
Several exams have been used in the evaluation of the COM, since XR, polytomography, three-dimensional computed tomography and magnetic resonance, but the high resolution computed tomography is the most common exam due to the anatomic information it provides (4).
The computed tomography (CT) of temporal bones demonstrates with large accuracy the presence of abnormal tissue in the middle ear, but cannot define whether this tissue with soft parts density represents or not the presence of a cholesteatoma. Nevertheless, when connected to osseous erosion of some structures like ossicular chain (Figure 1), tympanic tegmen (Figure 2), bony labyrinth (Figure 3) and lateral attic wall (Figure 1), etc., it is strongly indicative of cholesteatoma (5). The literature shows a sensitivity ranging from 70 (4) to 96% (6.7) for identification of the cholesteatoma in these cases. The CT is also crucial for the demonstration of the middle ear anatomy and possible complications such as fistulas of the lateral semicircular canal and tegmen or canal dehiscence of the facial nerve. The use of CT in the preoperative evaluation of the patient with chronic otitis media is still controversial nowadays. Some otologists use it regularly aiming to evaluate the extension of the disease, schedule the surgical technique to be adopted and identify potential scenarios of risk of complications (8, 9). Others reserve its utilization for cases of suspicion of complication, recurrence or diagnostic doubt, using the surgical indication only for the clinical profile presented (5, 10). The objective of this study is to connect clinical and radiological findings of patients with chronic suppurative otitis media to surgical and histopathological findings and to confirm a concordance of the surgical indication with the technique performed.
METHODRetrospective study through analysis of the record of all patients with diagnosis of chronic otitis media submitted to mastoidectomy surgery between the period of February, 2007 and September, 2008, in our service.
We included patients with diagnosis of chronic otitis media diagnosed based on the clinical profile of chronic purulent otorrhea without recovery from the suitable clinical treatment and who had perforation of the tympanic membrane, polyp in middle canal, retraction bag or cholesteatoma visible through otoscopy. And all patients described in the CT record of temporal bones were programmed for surgery.
We excluded patients submitted to surgery before (mastoidectomy review), as well as those who did not have such descriptions in the report.
The data collected were divided into three groups: closed mastoidectomy with tympanoplasty (with or without reconstruction of the chain), open mastoidectomy (with or without reconstruction) and subcortical mastoidectomy (with or without reconstruction).
We compared the clinical suspicion according to the findings described by otoscopy and tomography of cholesteatoma with the surgical and histopathological findings. The tomographic evaluation was considered to be indicative of cholesteatoma when presented soft parts density tissue in the middle ear connected to bone erosion. We also reviewed the presence of ossicular chain alterations (erosion, disjunction, fusion or displacement), erosion of the tympanic tegmen, the lateral semicircular canal and the facial nerve canal. In order to connect the CT findings concerning the presence of such finding we computed the sensitivity, specificity, positive predictive value and negative predictive value, individually, for all criteria assessed. The research project was approved by the Ethics Committee in Research of the Institution under the protocol CEP 2007/08.
RESULTSWe obtained eighty-four patients in the period, from whom six were excluded for having already been submitted to prior surgery for mastoidectomy review, and twenty had incomplete data regarding the CT, which prevented the inclusion to the tomographic findings connection to intraoperative findings, but they were analyzed as regards to other data.
As for sex, forty-two (53.8%) patients were of the female sex and thirty-six (46.2%) of the male sex. The mean age of the patients were of 33.9 years, ranging from three to sixty-six years old. Thirty-three (42.3%) patients had affection of the right ear, twenty-five (32.5%) of the left ear and twenty (20%) of both ears. Four (5.13%) patients had bilateral disease and were submitted to surgery in both ears in this period, summing up eighty-two ears analyzed.
Out of these ears, thirty-three (40.24%) had cholesteatoma, in three (3.65%) cases no cholesteatoma was viewed in the intraoperative, but it was seen in the histological analysis and in one case of cholesteatoma viewed from the intraoperative there was no confirmation from the histopathological analysis.
As regards to the clinical profile, fifty-two (63.41%) ears had intermittent otorrhea, twenty-seven (32.92%) had continuous otorrhea and three (3.65%) did not present any case of otorrhea (only hypacusis). The mean time of evolution of the disease was of thirteen years ranging from two months to fifty years. The presence of central perforation of the tympanic membrane (TM), marginal perforation of the TM, TM retraction bag, polyp in the external acoustic canal and white lamellar debris suggestive of cholesteatoma are connected to the confirmation of cholesteatoma in Table 1. In four patients, it was not possible to view adequately the TM in the preoperative exam due to an abundant purulent secretion and an inflammatory process. Some patients had associate alterations and the worst alteration was used for connection to the finding of cholesteatoma.
58 reports were analyzed with a total of sixty-two ears for connection between the findings of tomographic and intraoperative cholesteatoma. Table 2 shows the results found. For the finding of cholesteatoma, the CT presented 72.73% of sensitivity and 82.5% of specificity in the identification of the cholesteatoma. The positive predictive value was of 69.56% and the negative predictive value of 84.62%.
The findings of ossicular chain alterations connected to their suspicion in the CT are described in Table 3. The most frequent alteration found was the erosion of the anvil long reach, present in twenty-two cases (26.83%), which occurred separately in fourteen cases and connected to other alterations in eight cases. The CT presented a sensitivity of 56.67% and specificity of 84.37% in the identification of alterations to the ossicular chain. The positive predictive value was of 77.27% and the negative predictive value of 67.5%.
Table 4 shows the results of the presence of tympanic tegmen erosion. The sensitivity may not be evaluated because there was no case of tegmen erosion. The specificity of the exam was of 91.93% and the negative predictive value of 100%.
Table 5 shows the results of the presence of erosion of the lateral semicircular canal (LSC). The CT presented a sensitivity of 100% and specificity of 96.67% in the identification of erosion of the lateral semicircular canal. The positive predictive value was of 50% and the negative predictive value of 100%.
Table 6 presents the results of the presence of dehiscence of the facial nerve canal (FNC). In our study, seven patients had dehiscence of the facial nerve canal in its tympanic portion and no case was previously identified in the CT. The only suspect case had no alterations in the intraoperative approach. The specificity was of 98.18% and the negative predictive value was of 88.52%.
Fifty-six closed, nineteen open and seven subcortical mastoidectomy operations were carried out. The preoperative indication was altered in nine cases and: in three cases closed mastoidectomy was indicated with identification of cholesteatoma in the intraoperative approach and the choice was for open technique; in two cases open mastoidectomy was indicated for suspicion of cholesteatoma that was not confirmed in the intraoperative and the choice was for closed operation; in two cases closed mastoidectomy was indicated and subcortical technique was the choice, one case due to aditus ad antrum fibrotic block of difficult handling and another due to the presence of cholesteatoma restricted to the attic region; in two cases open mastoidectomy was indicated and the subcortical technique was adopted, one case due to restrict space for drilling not predicted in the preoperative exam and another due to a cholesteatoma limited to the attic region.
Table 7 shows the relationship between the surgical technique used and the presence of cholesteatoma. Closed mastoidectomy was adopted in nine cases of cholesteatoma. In six cases we opted for this technique because a cholesteatoma was identified limited to the attic region with full removal in the surgical operation. In three cases the cholesteatoma was only identified in the histopathological analysis.
The subcortical technique was previously indicated in three cases due to identification of low tegmen with restrict space for drilling by the usual technique.

Figure 1. Erosion of the spur and hammer.
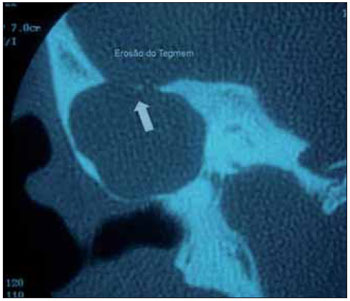
Figure 2. Tegmen erosion.
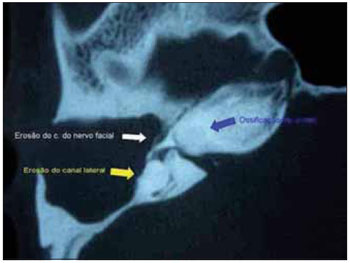
Figure 3. Erosion of the lateral canal, facial nerve canal and cochlea ossification.
We presented a series of seventy-eight patients with diagnosis of chronic suppurative otitis media, operated for the first time, in a period of one year and seven months, which indicated a high prevalence of this disease in our population.
The CSOM was present in 40.24% of the ears analyzed. This high rate of CSOM may be connected to the long time of evolution in most cases, since the continuum theory suggests the alterations in the middle ear occur progressively with CSOM as their last consequence (11). Out of thirty-three cases, three were identified only in the histopathological analysis. The cholesteatoma may have been too small or not correctly identified in the intraoperative approach, but we believe epithelial remains were sent along with the inflammatory material and incorrectly interpreted as cholesteatoma by the pathologist. But as we cannot identify what occurred, we opted to assume these cases as CSOM and perform a more detailed follow up in such cases, since closed mastoidectomy was used for these patients. In one case, the cholesteatoma was viewed in the intraoperative approach, but there was no histopathological confirmation. This probably occurred because of inadequate or insufficient forwarding of material for analysis or error in the pathologist diagnosis.
The occurrence of white lamellar debris in all cases was connected to the presence of cholesteatoma, but it was the most seldom alteration found in only 8.5% of all ears analyzed. As this classic alteration was rarely found in our study, we believe in the importance of the clinical and radiological correlation (clinical history) for the evaluation of the presence of the cholesteatoma (12,13).
The literature shows sensitivity for CT ranging from 70 to 96.88% (average of 85%) ( 10, 12,18). In our study, the CT sensitivity in detecting the cholesteatoma was of 72.73%.
The CT had a sensitivity of 56.67% in the detection of alterations in the ossicular chain. The alterations found were: medial displacement of the chain, fusion and hardening of the chain and erosion. The most common alteration was the erosion of the anvil long reach, which is compatible with the literature (10, 14, 15, 16, 17, 18, 19).
The sensitivity was variable, according to the alterations, ranging from 50% in the anvil isolated erosion identification to 100% when there was erosion of the three ossicles. The case that presents isolated erosion of the hammer had a partial erosion of the hammer head and it would be difficult to be viewed in the CT. The literature presents similar results, with sensitivity ranging from 50 to 100% (6, 8, 10, 12, 14, 17, 18).
We note associate erosions are more easily identified and the isolated erosions, especially those of the stirrup, are more difficult to identify (6, 10, 12, 18). In our study only one case had stirrup isolated erosion, but it was in the group of patients who had no suitable data regarding the CT.
There was tomographic suspicion of tegmen erosion in five patients, but no patient had such alteration in the intraoperative approach. The specificity was 91.93%, similar to that described in the literature (12, 14, 18). The works show that when there is tegmen erosion there is a high sensitivity in its identification. However, a high number of false-positive cases occur (4, 6, 8, 10, 12, 14, 18). This may be explained by the CT technique artifacts because as these are a fine osseous lamina and the tomographic cuts vary from 0.5 to 2mm, images of this section are aggregated and may lead to a false impression of the tegmen dehiscence. The same occurs with other structures like the lateral semicircular canal and the facial nerve canal. Some authors recommend the performance of MR for investigation of the suspect cases, because through this method it is possible to evaluate with major accuracy the intracranial extension of a cholesteatoma or the presence of meningocele or tympanic meningoencephalocele (3, 5, 15).
The lateral semicircular canal erosion was present in two cases and was correctly identified in the CT. There were two false-positive cases and the exam presented a specificity of 96.67%. The literature shows similar findings and the exam offers a high sensitivity for detection of such alteration, ranging from 85% to 100%, but the false-positive cases are frequent for the same reason as mentioned above. We identified seven cases of the facial nerve canal dehiscence in its tympanic segment, but there was no previous tomographic suspicion. In only one case there was suspicion of such alteration, which was not confirmed in the intraoperative approach. The works in the literature show variable results, since results like ours, of no case identified, up to high sensitivity of 94.1% (6, 7, 14, 17, 18). Most authors report a low sensitivity in the detection of the facial nerve canal dehiscence and many false-positive cases. We believe that in spite of the low sensitivity described in the literature, many of these cases could be identified in the CT, but the radiologists were not enough precise in their identification, and as the historic reports are concise as for the CT alterations, we may not infer whether the surgical staff identified such alterations previously. As the facial nerve canal dehiscence is a frequent alteration that may be present in up to 55% of the normal temporal bones (4), and the CT offers a low sensitivity for detection of such alteration, we must always act very carefully in the manipulation of areas close to the facial nerve to prevent iatrogenic lesions.
Most surgeries performed were closed mastoidectomy (68.29%), followed by the open mastoidectomy (23.17%) and subcortical mastoidectomy (8.54%). In our service, we opted for the operation of the open technique in most cases of cholesteatoma, but as we could make the full removal of the small cholesteatoma restricted to the aditus in six cases, the closed technique was used. As mentioned above, three cases of closed technique, in which no cholesteatoma was noted in the surgical operation, allowed a positive histopathological analysis for cholesteatoma. The subcortical technique was adopted in seven cases, which was previously indicated in three of them due to the tomographic findings, and in four cases due to the already mentioned surgical findings. We altered our prior surgical indication in only 10.97% of the cases. BANERJEE et al (8) also connected the prior radiological evaluation to the influence of the surgical indication with similar results, by showing a good correlation between the surgical indication, evaluation of the extension of the disease and presence of cholesteatoma.
They also noticed the CT had no safe results as regards to the presence of possible risk situations, like the facial nerve canal dehiscence, for instance. The previous radiological evaluation contributed critically for indication of the technique to be used, by predicting technical difficulties such as restrict space for drilling due to a dura mater of the low middle cavity, for example, and predicting the presence of cholesteatoma. Nevertheless, the exam has limitations for evaluation of other risk situations like dehiscence of the facial nerve canal and lateral semicircular canal and we should beware even faced with a normal exam.
It is essential to be able to predict if there is cholesteatoma and the technique to be used because we may select more urgent cases, schedule the surgical program in a better way and inform the patient with more precision as regards to the procedures to be employed and the prognosis. However, as in about 10% of the surgeries there may be a change of procedure, we must always alert the patients as for the procedures and the results that may come.
We will keep on using routine radiological evaluation in the cases of chronic suppurative otitis media for the above mentioned reasons. We understand the exam offers diagnostic limitations but serves as one more instruments for evaluation that helps the surgical programming and a better understanding of the middle ear anatomy of each patient.
CONCLUSIONIn our study we notice the otoscopy findings show a good correlation with the presence of cholesteatoma in the intraoperative approach.
The correlation of tomographic findings described a good sensitivity for detection of the presence of cholesteatoma and of lateral semicircular canal erosion. It presented a good sensitivity for identification of large erosions of the ossicular chain but not in the identification of isolated erosions. The exam could not identify any case of dehiscence of the facial nerve canal.
The clinical and radiological evaluation was important for indication of the surgical technique to be used, with a low rate of alteration to the procedures, faced with the intraoperative findings.
BIBLIOGRAPHICAL REFERENCES1. Fritz P, Rieden K, Lenarz T, Haels J, Winkel K. Radiological evaluation of temporal bone disease: highresolution computed tomography versus conventional Xray diagnosis. Br J Radiol. 1989, 62(734):1071-3.
2. Chul HJ, Wang PC. Preoperative evaluation of bone destruction using threedimensional computed tomography in cholesteatoma. J Laryngol Otol. 2004, 118(10):827-9.
3. Maroldi R, Farina D, Palvarini L, Marconi A, Gadola E, Menni K, Battaglia G. Computed tomography and magnetic resonance imaging of pathologic conditions of the middle ear. Eur J Radiol. 2001, 40(2):78-93.
4. Blevins NH, Carter BL. Routine preoperative imaging in chronic ear surgery. Am J Otol. 1998, 19 (4):5273-5.
5. Leighton SE, Robson AK, Anslow P, Milford CA. The role of CT imaging in the management of chronic suppurative otitis media. Clin Otolaryngol Allied Sci, 1993, 18(1):23-9.
6. Gaurano JL, Joharjy IA. Middle ear cholesteatoma: characteristic CT findings in 64 patients. Ann Saudi Med. 2004, 24(6):442-7.
7. Chee NW, Tan TY. The value of preoperative high resolution CT scans in cholesteatoma surgery. Singapore Med J. 2001, 42(4):155-9.
8. Banerjee A, Flood LM, Yates P, Clifford K. Computed tomography in suppurative ear disease: does it influence management? J Laryngol Otol. 2003, 117(6):454-8.
9. Schuring AG. Cholesteatoma and imaging. Am J Otol. 1991, 12(5):394-5.
10. Jackler RK, Dillon WP, Schindler RA. Computed tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope. 1984, 94(6):746-52.
11. Yoon TH, Paparella MM, Schachern PA, Lindgren BR. Morphometric studies of the continuum of otitis media. Ann Otol Rhinol Laryngol Suppl. 1990, 148:23-7.
12. Garber LZ, Dort JC. Cholesteatoma: diagnosis and staging by CT scan. Cholesteatoma: diagnosis and staging by CT scan. J Otolaryngol. 1994, 23(2):121-4
13. Twemlow S. Computerised tomography: its role in the assessment of ear disease. Radiogr Today. 1991, 57(648):22-6.
14. Sneyers W, Debruyne F, Morlion J, Lemahieu F, Baert A. Cholesteatomas of the temporal bone: a comparison of CT and operative findings. Acta Otorhinolaryngol Belg. 1991, 45(4):369-73.
15. Yates PD, Flood LM, Banerjee A, Clifford K. CT scanning of middle ear cholesteatoma: what does the surgeon want to know? Br J Radiol. 2002, 75(898):847-52.
16. Watts S, Flood LM, Clifford K. A systematic approach to interpretation of computed tomography scans prior to surgery of middle ear cholesteatoma. J Laryngol Otol. 2000, 114(4):248-53.
17. OReilly BJ, Chevretton EB, Wylie I, Thakkar C, Butler P, Sathanathan N, Morrison GA, Kenyon GS. The value of CT scanning in chronic suppurative otitis media. J Laryngol Otol. 1991, 105 (12):990-4.
18. Park KH, Park SI, Kwon J, Kim YM, Park IY, Sung KJ. Highresolution computed tomography of cholesteatomatous otitis media: significance of preoperative information. Yonsei Med J. 1988, 29(4):367-72.
19. Jeng FC, Tsai MH, Brown CJ. Relationship of preoperative findings and ossicular discontinuity in chronic otitis media. Otol Neurotol. 2003, 24(1):29-32.
1 Resident Doctor.
2 Doctoral Degree from UNIFESP. Professor of the medical school of ABC, Coordinator of the Otorhinolaryngology residence of the State Hospital of Diadema.
3 Master's Degree in otorhinolaryngology from UNIFESP. Otorhinolaryngologist and Supervisor of the medical residence of the State Hospital of Diadema.
4 Otorhinolaryngologist from UNIFESP. Fellowship in Otology from UNIFESP.
Institution: UNIFESP/EPM - Universidade Federal de São Paulo / Escola Paulista de Medicina. São Paulo / SP - Brazil. Mail address: Anelise Abrahao Salge Prata - Rua Pedro de Toledo, 947 - 2º andar - Vila Clementino - São Paulo / SP - Brazil - Zip code:04039-002 - Telephone: (+55 11) 5539-5378 - E-mail: anelise_asp@yahoo.com.br
Article received on October 10, 2010. Approved on December 10, 2010.